This article is written by medical professional Dr Yuri Ochiai
What is endometriosis
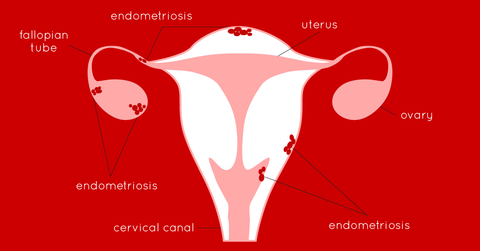
Endometriosis is an inflammatory disease in which tissue similar to the lining of the uterus grows outside the uterus.
Normally, the endometrium thickens in preparation for potential pregnancy and sheds during menstruation if pregnancy does not occur. However, in endometriosis, this tissue implants grows on other pelvic organs, such as the ovaries, fallopian tubes, and the outer surface of the uterus. This abnormal tissue responds to hormonal changes in the menstrual cycle, leading to inflammation, scarring, and the formation of adhesions.
It is the most common cause of chronic pelvic pain in women, painful menstruation and infertility. Is a complex syndrome characterized by a chronic inflammatory process that affects primarily pelvic tissues, including the ovaries. It is caused when shed endometrial tissue travels retrograde into the lower abdominal cavity.
Endometriosi is a word derived from the Greek endo ‘'inside'', metra ''uterus'' and osis ‘' disease,''. Most frequently, endometrial tissue is found in ovaries but it can also be found in the fallopian tubes, uterosacral ligaments and the gastrointestinal tract.
Endometriosis signs and symptoms
Endometriosis-related symptoms can affect a woman’s overall health and mental and social well-being. It can cause a significant deterioration in the quality of life. In 66% of women with endometriosis, the first symptoms of the disease appear before the age of 20 [32]. Symptoms of endometriosis include:
1- Pain
- gradually increasing acute premenstrual;
- pelvic: this pain may vary in intensity and typically worsens just before and during menstruation. It can also occur during ovulation or at other times throughout the menstrual cycle. In very severe cases, pain can be present during the whole menstrual cycle;
- sacral region of the spine wich can be confused for a musculoskeletal pain coming from the lumbar region;
- menstruation with severe cramps (dysmenorrhea);
- during or after sexual intercourse (dyspareunia);
- during defecation;
- during urination;
- radiating to the back.
2- Abundant irregular menstruation
3- Diarrhea or constipation
4- Infertility
5- Chronic fatigue
6- GI symptoms
Like other inflammatory diseases, many patients may also present with gastrointestinal symptoms such as bloating, abdominal pain and changes in stool. This symptoms may hide a celiac disease or non celiac gluten intolerance that can also be linked to endometriosis. Other pathologies linked to gut dysbiosis are SIBO, candida, food sensitivities, leaky gut, etc.
Because of all the mentioned symptoms above, some patients suffer from pain almost everyday of their menstrual cycle making their daily life very hard. Others that don’t have the possibility to rest or avoid some of their duties, have to take high doses of painkillers.
How common is endometriosis
It affects around 5-10% of women in their reproductive years - translating to 176 million women worldwide.
The risk of developing endometriosis is the lowest in black women, the highest in Asian women. Caucasian women have a higher risk of getting sick than black women [26].
Nowadays, a lot of women often remain asymptomatic and go undiagnosed. Endometriosis is estimated to affect up to 70% in women with chronic pelvic pain.[14] In the U.S., 11.2% of all women between 18 and 45 years old hospitalized for genitourinary causes were diagnosed with endometriosis, and approximately
10.3% of the women who have undergone gynecologic surgeries have endometriosis.[15]
The diagnosis of endometriosis in the majority of women is often delayed, and thus, women unavoidably suffer from the pain and the long-term effects of this debilitating disease, including infertility. In women with infertility, endometriosis has been found to be up to 50%.
How is endometriosis diagnosed
Diagnosis of endometriosis is usually done on the basis of clinical history since most women show normal results of physical examination. Despite the range of blood tests that have been evaluated, a reliable blood test marker has yet to be identified for the diagnosis of endometriosis.
Therefore, the use of transvaginal and transabdominal ultrasound is a useful tool to detect pelvic masses. Transvaginal ultrasound is used to better visualize endometrium and uterine cavity and detect ovarian endometriotic cysts (endometrioma) but does not rule out peritoneal endometriosis, endometriosis-associated adhesions and deep infiltrating endometriosis [66–70]. Occasionally, a magnetic resonance imaging and computed tomography scans are conducted to characterize the pelvic masses.
It is important to point out that the ultrasound needs to be made by a professional with expertise in detecting ovarian cysts and endometriosis otherwise endometriosis might be undiagnosed.
Despite the aforementioned tentative tests available, most approved confirmatory diagnosis of endometriosis is laparoscopic inspection with biopsy [66].
During this minimally invasive surgical procedure, a thin, lighted tube (laparoscope) is inserted through a small incision in the abdominal wall. The laparoscope allows direct visualization of the pelvic organs, including the uterus, ovaries, fallopian tubes, and peritoneum (lining of the pelvis). If endometriosis is suspected or confirmed during the procedure, tissue samples (biopsies) may be taken for histological confirmation. Laparoscopy also allows for the assessment of the extent, location, and severity of endometriotic lesions.
Staging of Endometriosis: If endometriosis is confirmed, it may be staged based on its extent and severity. The American Society for Reproductive Medicine (ASRM) has established a classification system ranging from stage I (minimal) to stage IV (severe) based on the findings during surgery.

Treatment for endometriosis
Pain Medications
Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or naproxen, can help relieve pelvic pain and menstrual cramps. Prescription pain medications, including stronger NSAIDs or opioids, may be considered for more severe pain. Hormonal Therapy Hormonal therapies aim to suppress or reduce the growth and activity of endometrial tissue outside the uterus. These treatments can provide relief from pain and slow the progression of endometriosis. Common hormonal therapy options include: Oral Contraceptives (Birth Control Pills): These can help regulate the menstrual cycle, reduce pain, and prevent the progression of endometriosis.
* Progestin-Only Therapy: Progestin-containing medications, such as progestin-only birth control pills, intrauterine devices (IUDs), or injections, can help suppress endometrial tissue growth.
* Gonadotropin-Releasing Hormone (GnRH) Agonists: These medications induce a temporary state of menopause by suppressing the production of estrogen, which can help alleviate symptoms and reduce endometrial
* Danazol: An androgenic medication that can suppress endometrial tissue
Surgical Intervention
Surgery may be recommended in cases of severe endometriosis or when other treatments are ineffective. Surgical options include:
* Laparoscopic Excision: Minimally invasive surgery to remove endometrial tissue growths, adhesions, and cysts while preserving healthy tissue.
* Laparoscopic Ablation: A procedure that uses heat or laser to destroy endometrial tissue. This is the best option for all women with endometriosis because it has less recurrence than the excision technique.
* Hysterectomy: Removal of the uterus is considered a last resort when all other treatments fail or when the disease is In some cases, the ovaries and fallopian tubes may also be removed (salpingooophorectomy). This surgery won’t heal your endometriosis. Is just an option if you have adenomyosis and non manageable treatment.
Holistic treatment
* Diet: avoid inflammatory ingredients such as processed foods, sugar, alcohol, cow dairy, grains and gluten specially the week before the period.
* Exercise: prioritize strength exercise at least 2-3 times a Try to walk, bike or move as much as you can during the rest of the week.
* Avoid toxics and endocrine disruptors present in many cosmetic, beauty and cleaning products.
* Detox techniques such as sauna or dry brushing are useful in women who have been exposed to toxins such as pollution, mercury fillings, environmental chemicals like pesticides, etc.
* Liver support: certain foods can help the liver like sulphur rich veggies, broccoli, cauliflower, etc. Intermittent fasting can help too.
* Address any trauma, emotional distress that you are going Mental health and well being will be a crucial part of the healing process. Try meditation or consult a psychologist if needed.
* Physical therapy, osteopathy, acupuncture, and relaxation techniques may help manage pain and improve quality of life for some individuals.
* Other helpful therapies are Mayan Womb Massage, Cranial Sacral Vaginal Steaming Trauma Release Work
References:
https://pubmed.ncbi.nlm.nih.gov/30994890/
https://www.ncbi.nlm.nih.gov/books/NBK567777/ https://pubmed.ncbi.nlm.nih.gov/30026507/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8508982/ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5737931/
https://www.who.int/news-room/fact-sheets/detail/endometriosis
 Your Account
Accedi
Your Account
Accedi
 Basket
Basket

